Provider Alert! Medicaid drug formulary changes effective 1/30/2020
The Texas Vendor Drug Program (VDP) will implement changes to the state Medicaid drug formulary, effective Thursday, January 30, 2020. Select medications will be moving from “preferred” to “non-preferred” status and vice-versa. Texas Children’s Health Plan wanted to notify you in advance so that these changes do not impact the ability of your patients to obtain their medications. A summary of the changes is included below.
Preferred and non-preferred medications may continue to require clinical prior authorizations. In addition to any clinical prior authorization requirements, non-preferred medications will also require a “step therapy prior authorization.” This means that members must have attempted and failed at least one preferred medication before obtaining a non-preferred medication. The preferred drug list (PDL) can be found on the VDP website: https://www.txvendordrug.com/formulary/prior-authorization/preferred-drugs. Medicaid managed care plans are required to follow the PDL.
Preferred drugs are medications recommended by the Texas Drug Utilization Review Board for their efficaciousness, clinical significance, cost effectiveness, and safety. Texas Children’s Health Plan encourages providers to initiate a preferred medication to members new to therapy. When possible, Texas Children’s Health Plan also encourages switching existing members to a preferred agent. Texas Children’s Health Plan will provide an exception to the step therapy requirement for existing members utilizing Saphris (asenapine) who are stable on therapy. These members will not have to switch to a preferred medication if their existing prior authorization approval expires.
If you have questions, please contact us at tchppharmacy@texaschildrens.org.
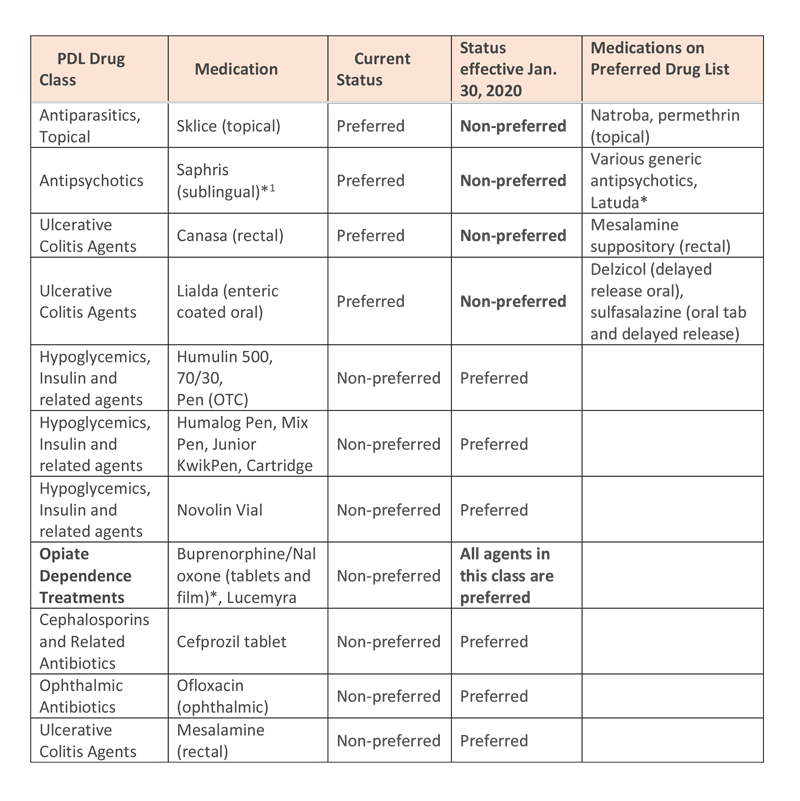
[1] Members who are stable and currently using Saphris can continue therapy after January 30, 2020. These select members will not have to switch to a preferred medication if their existing prior authorization expires.
*All medications marked with an asterisk will continue to require a Prior Authorization in addition to preferred or non-preferred medication status.





Leave a Reply
You must be logged in to post a comment.