Provider Alert! Clarifying Information on Provider Enrollment and Management System (PEMS)
Date: May 18, 2023
Attention: All Providers
Master Provider File effective date: To Be Determined
Important provider notice: As a reminder, the Provider Enrollment and Management System (PEMS) is the required Texas Medicaid & Healthcare Partnership (TMHP) program which is the single tool for provider enrollment, reenrollment, revalidation, and maintenance requests (maintaining and updating provider enrollment record information) for Texas Medicaid. Clarifying information on PEMS can be found here: https://www.tmhp.com/news/2023-05-16-provider-enrollment-and-management-system-pems-post-deployment-update
Providers are strongly encouraged to visit this site for an overview of the most current PEMS information.
Some topics with clarifying information include the following:
- Updating CLIA Certifications in PEMS- Providers must update their Clinical Laboratory Improvement Amendment (CLIA) certifications in PEMS under the License/Certification/Accreditation link. Providers may find more information about updating CLIA certifications in PEMS on the Licenses/Certifications/Accreditations page on tmhp.com.
- PEMS Multi-Factor Authentication for Electronic Funds Transfer (EFT) Updates- Effective April 15, 2023, additional verification is required for PEMS EFT (electronic fund transfer) changes. A personal identification number (PIN) sent to the email address on file will be needed to make any changes to EFT information. EFT change requests cannot be created within 30 calendar days after approval of a “Maintenance-Provider Information-Change Email” request.
As an MCO, TCHP will contract, credential and pay only those providers who are properly enrolled with TMHP and whose information is received in the official PEMS file from TMHP. In addition, it is important that every provider be enrolled at each location where they see patients. This is to help ensure claims process correctly.
UPDATE on guidance for practice location and license:
- When a user adds a program/practice in PEMS and the program/practice matches another program/practice at the same location, the following message will display: “Unable to save a duplicate program record. Please reenroll the Program record with the same Program and Primary Taxonomy or change the Program and Primary Taxonomy to be different than the other duplicate Program record.”
- PEMS will only allow physical addresses (not P.O. boxes) to be added as a practice location on the Practice Location Information page and on the Ownership/Controlling/Principal Information page in PEMS.
- On the Program and Services Participation Details page, providers now have the option to remove the Licenses/Certifications/Accreditations that are applied to the program practice record. This will end date the license association to the program practice for licenses that have previously been approved and will display the association’s effective dates for the segments as “Removed.” Licenses that have not been approved and that were added by mistake will not have the termination date added.
For your convenience we have included information on PEMS enrollment, provider requirements, and retro-active billing allowances at the end of this Provider Alert.
Resource: https://www.tmhp.com/topics/provider-enrollment
Resource: https://www.tmhp.com/news/2023-01-30-provider-enrollment-and-management-system-pems-post-deployment-update
How PEMS is accessed: PEMS is accessed through My Account. PEMS access is connected to the National Provider Identifier (NPI) or Atypical Provider Identifier (API) associated with the TMHP user account. Providers should ensure that the NPI has all the current and correct information. After a TMHP user account is created, follow these best practices for account management:
- Assign at least two administrators.
- Update user permissions as staff changes occur.
- Look for reminders for upcoming enrollment tasks on the Message Dashboard.
UPDATE on guidance for PEMS Enrollment Deficiencies: Providers have a total of 45 business days to complete and resolve all deficiencies when completing their enrollment application. PEMS will display the message “You must respond to and resolve all deficiencies within 45 business days.”
More information on provider enrollment identification:
- PEMS basis each enrollment application on the applying provider’s NPI or API.
- Providers who would like to enroll in Texas healthcare programs must do so under one of two categories, individual or organization, determined by their NPI or API.
More information on NPI:
- Individual providers, performing providers, and sole proprietors will enroll in PEMS with an NPI type of Individual.
- Facility and group healthcare providers who have a single employee or thousands of employees will enroll in PEMS with an NPI type of Organization.
- NPIs are obtained from the National Plan and Provider Enumeration System (NPPES).
More information on API:
- Providers or individuals who do not provide healthcare services and are not required to have NPIs may have been issued APIs. These providers should use their APIs for enrollment purposes. Resource: https://www.tmhp.com/topics/provider-enrollment/pems/npi-type-and-program-selection
Provider Requirements
Providers can view and confirm their revalidation date and enrollment information in PEMS here. As a reminder, effective May 11, 2023, the federal flexibility to extend Medicaid provider revalidation dates that were due during the federal COVID-19 PHE has ended.
UPDATE on guidance for revalidation dates: TMHP has sent an email to affected providers with a recalculated revalidation due date. Providers can find their revalidation due dates in the Provider
Dashboard in PEMS under the Revalidation Due Date field in the Enrollment Information section of the Provider Information page. To reduce application time, we encourage providers to have the following information available:
- First and last name
- Organization name
- Social Security number
- Date of birth
- Employer’s Tax Identification Number and legal name
- Licenses or certifications, if applicable
- Identification for the provider and any person who meets the definition of owner, creditor, principal, subcontractor, or managing employee
- Documentation related to disclosures, if needed
Providers revalidating an existing enrollment should continue to submit claims to meet their timely filing requirements. For provider enrollment help, click here.
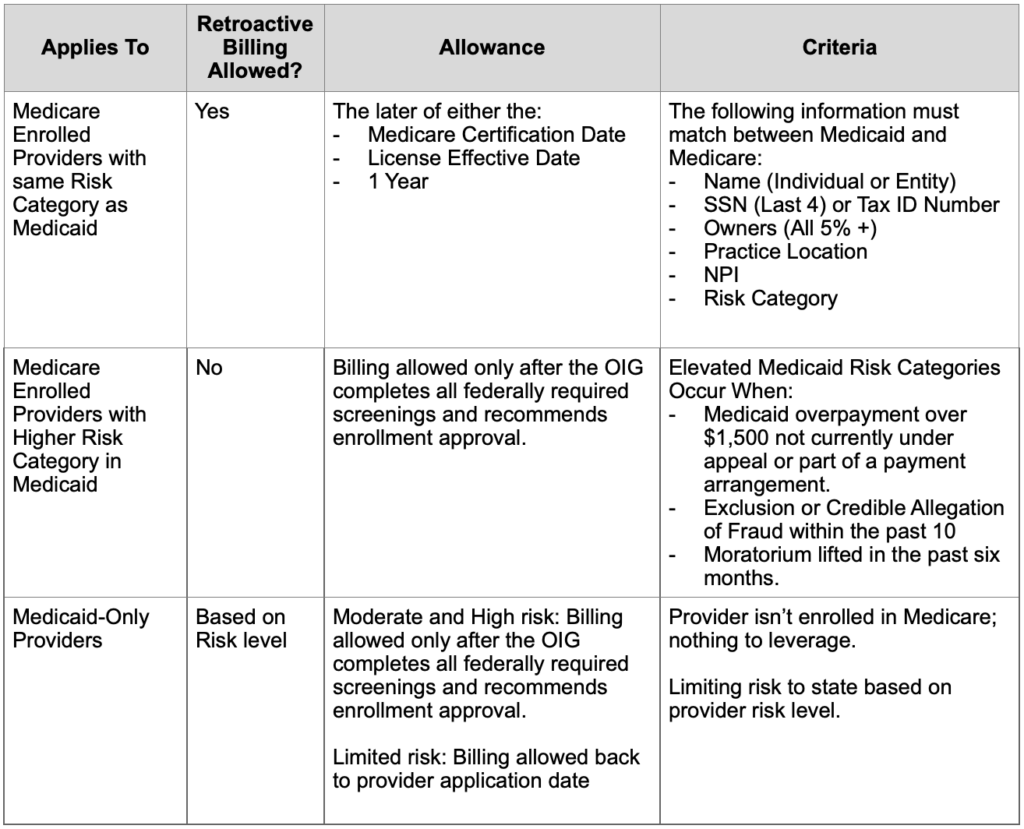
Provider effective dates: Prior to the PEMS implementation, the provider billing effective date could be the Medicare enrollment effective date, the provider license date, or the application completion date (retroactive billing date).
With PEMS implementation, new and reenrolled provider agreement effective dates were upon signature of the agreements and required all screenings to be completed. After further review, HHSC, in collaboration with the Office of Inspector General (OIG) made the decision to allow retrospective billing effective dates in certain circumstances, as outlined in the table below.
Retroactive Billing Allowances Table
If you have any questions, please email Provider Relations at: providerrelations@texaschildrens.org.
For access to all provider alerts, log into: www.thecheckup.org or www.texaschildrenshealthplan.org/for-providers.